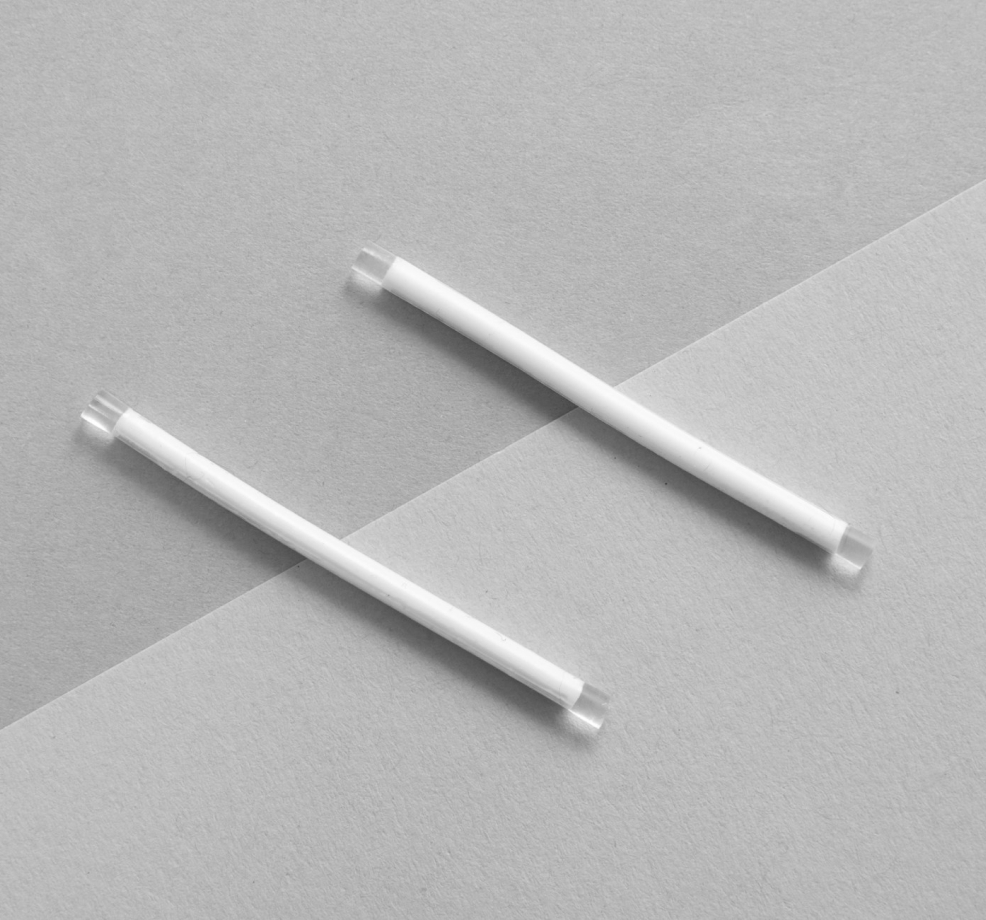
Implanon is a small, thin, plastic rod that is inserted under the skin of your upper arm. The rod releases small amounts of the hormone progestogen which prevents pregnancy by (1) thickening mucus in the cervix so sperm cannot enter the uterus and (2) preventing ovulation (release of eggs from the ovaries). It is also important to note that Implanon does not protect against STIs.
Implanon is 99.9% effective and designed to stay in place for up to 3 years. It is reversible and return to fertility is rapid. Some women experience very light or no periods at all when on Implanon.
The most common side effect of Implanon is changes to the pattern of vaginal bleeding, such as irregular bleeding and prolonged light or heavy bleeding.
Implanon is not recommended for patients with a history of breast cancer. If you are experiencing unexplained vaginal bleeding, your doctor will first investigate this before the Implanon insertion.
Implanon insertion is a small procedure done by your doctor. A local anaesthetic will be used to numb the area before inserting the rod the skin on the inside of your arm. It is normally inserted during the first five days of the menstrual cycle. You may experience some bruising, itching, or soreness in your arm at the site of the implant following insertion or removal.

An intra-uterine device (IUD) is an effective and long-lasting form of contraception. It is a small, T-shaped device that is placed inside the uterus. There are two types of IUDs available in Australia – the copper IUD and the hormonal IUD (also known as the Mirena or Kyleena). Both are more than 99% effective at preventing pregnancy.
The IUD will be inserted by your doctor. First, your doctor will carefully explain the procedure to you, including what to expect during and after the insertion. Feel free to discuss any questions or concerns at this point. The insertion involves placing the IUD into the uterus through the cervix. When the IUD is in place, a string comes out through the cervix into the top end of the vagina. The string can be used to check if the IUD is still in place and helps with removal of the IUD by your doctor.
The copper IUD is a small T-shaped plastic device wrapped with fine copper wire. It works by (1) preventing sperm from fertilising the egg and (2) changing the lining of the uterus to make it less suitable for pregnancy.
As a long-term contraceptive option, the copper IUD is designed to stay in place for up to 10 years. It is reversible and return to fertility is rapid. It is a suitable option for women who are unable to use a hormonal form of contraception, as well as women who are breastfeeding.
Women can experience heavier and longer periods with the copper IUD. There is a very small chance of developing a pelvic infection at the time of IUD insertion and usually happens in the first 3 weeks after insertion.
The copper IUD should not be used if you could be pregnant, have a current pelvic infection, are experiencing unexplained vaginal bleeding, or are awaiting treatment for cervical cancer.

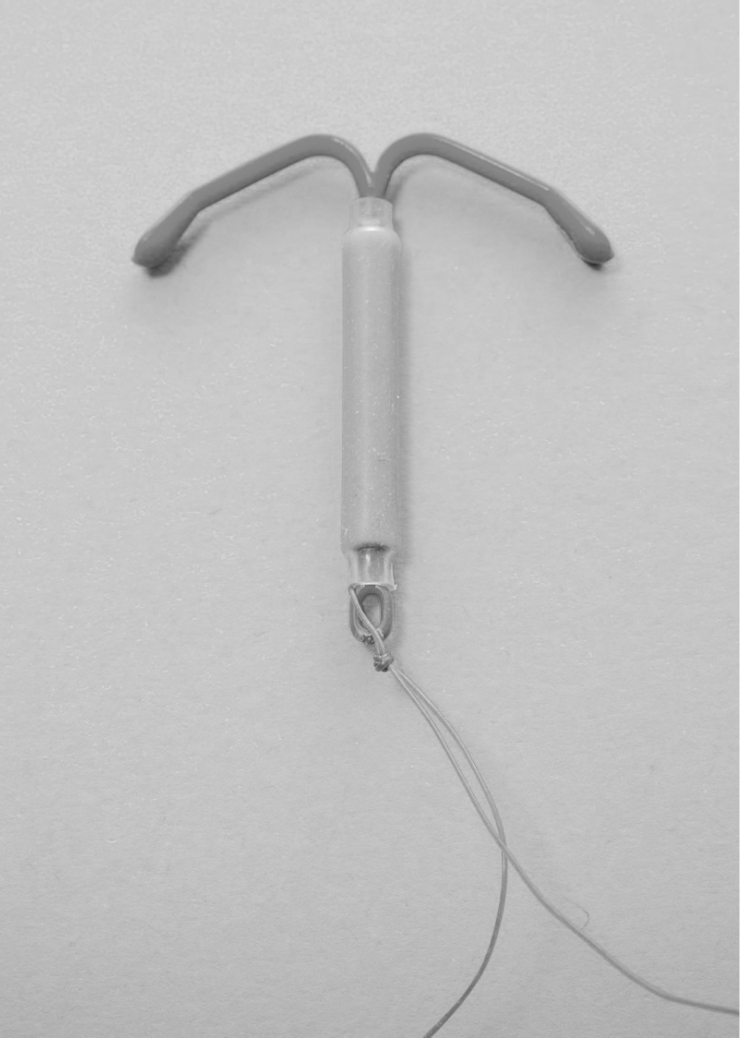
The hormonal IUD, also known as Mirena, is a small T-shaped device containing the hormone levonorgestrel. It works by (1) thickening cervical mucus to prevent sperm from entering the uterus and (2) prevents sperm from fertilising the egg.
As a long-term contraception option, the hormonal IUD is designed to stay in place for up to 5 years. It is reversible and return to fertility is rapid. For women experiencing heavy periods, the hormonal IUD is a great option as it makes bleeding lighter and may stop periods altogether.
In the first few months after insertion, some women may experience irregular bleeding or spotting. But this usually settles down over time and periods become shorter and lighter. There is a very small chance of developing a pelvic infection at the time of IUD insertion and usually happens in the first 3 weeks after insertion. The IUD may also be pushed out of the uterus, known as expulsion.
The hormonal IUD should not be used if you could be pregnant, have a current pelvic infection, are experiencing unexplained vaginal bleeding, or are awaiting treatment for cervical cancer.
Your doctor will take a thorough medical history and discuss contraceptive options that are most suitable for your individual circumstances.
